Traumatic Brain Injury (TBI)
Symptoms, Causes, Treatments, Recovery & Outlook
Understanding Traumatic Brain Injury
A Traumatic Brain Injury (TBI) is damage to the brain caused by an external force – usually a violent blow or jolt to the head or body. It can also occur if an object penetrates the skull and enters brain tissue (for example, a bullet or shrapnel). Essentially, the brain gets shaken or injured inside the skull. TBIs range widely in severity: a mild TBI, often called a concussion, might cause temporary symptoms, while a severe TBI can result in long-term problems with movement, thinking, or even coma and life-threatening complications.
To put it simply, imagine the brain as soft Jell-O inside a hard skull. If you hit your head hard or the head moves rapidly and then stops (like in a car crash), the brain can bounce or twist inside, leading to bruising, bleeding, or tearing of brain fibers. Even a “mild” brain injury is serious – there’s no such thing as “just a concussion” without importance, since it is a brain injury and needs care. According to the CDC, TBIs contribute to a significant number of disabilities and deaths every year. Common causes include falls, car accidents, sports injuries, and assaults (we’ll detail these shortly).
Traumatic brain injuries are a major public health concern. Children and older adults are especially vulnerable to falls; young adults and males have high rates of TBI from risky activities and sports. War and combat have also unfortunately made TBI a frequent injury among soldiers due to blasts and explosions. The effects of a TBI can be temporary or permanent and can affect physical abilities, thinking and memory, emotions, and behavior. Early recognition and prompt medical treatment of brain injuries improve outcomes, and rehabilitation can help individuals regain function and independence.
Symptoms and Severity Levels
TBI symptoms can appear immediately or develop over hours to days after the injury. They also vary based on injury severity. Doctors often classify TBIs as mild, moderate, or severe. Here’s what that typically means:
Mild TBI (Concussion): This is the most common type. It might involve a brief loss of consciousness (from a few seconds up to a few minutes) – but many concussions do not cause someone to black out at all. Instead, a person may be dazed, confused, or “see stars.” Symptoms of a mild TBI can include: headache, dizziness or balance problems, nausea or vomiting shortly after the injury, fatigue or drowsiness, blurry vision, ringing in the ears, and sensitivity to light or noise. The individual might have trouble concentrating or remembering things, feel foggy, or be irritable (cognitive and mood symptoms). They might also sleep more or less than usual or have difficulty sleeping. These symptoms are usually temporary, but even a mild TBI needs rest and monitoring because on rare occasions complications can develop. For example, a “brain bleed” could initially seem like a mild concussion and then worsen, so it’s important to watch for any worsening signs (like increasing headache, repeated vomiting, confusion, difficulty waking up).
Moderate to Severe TBI: These injuries involve more significant brain damage. They often (but not always) include a loss of consciousness that lasts longer – several minutes to hours in severe cases. Symptoms of moderate/severe TBI can encompass any of the mild symptoms plus more serious ones, such as: persistent or worsening headache (e.g., a headache that won’t go away or gets worse over time), repeated vomiting or nausea, convulsions or seizures, clear fluids draining from the nose or ears (this can indicate a skull fracture with leaking cerebrospinal fluid), profound confusion and disorientation, agitation or aggressive behavior (acting strangely combative or very restless), slurred speech, weakness or numbness in the extremities (like difficulty moving an arm or leg), loss of coordination, and unequal or dilated pupils in the eyes. In severe TBIs, the injured person might fall into a coma or another state of impaired consciousness (like not responding normally).
Infants and young children with TBIs might not be able to communicate their symptoms, so you look for signs like persistent crying, inability to be consoled, refusal to eat or nurse, unusual sleep pattern or irritability, or loss of interest in favorite toys. A baby might just be very lethargic or vomit repeatedly after a head injury – those are red flags to seek immediate care.
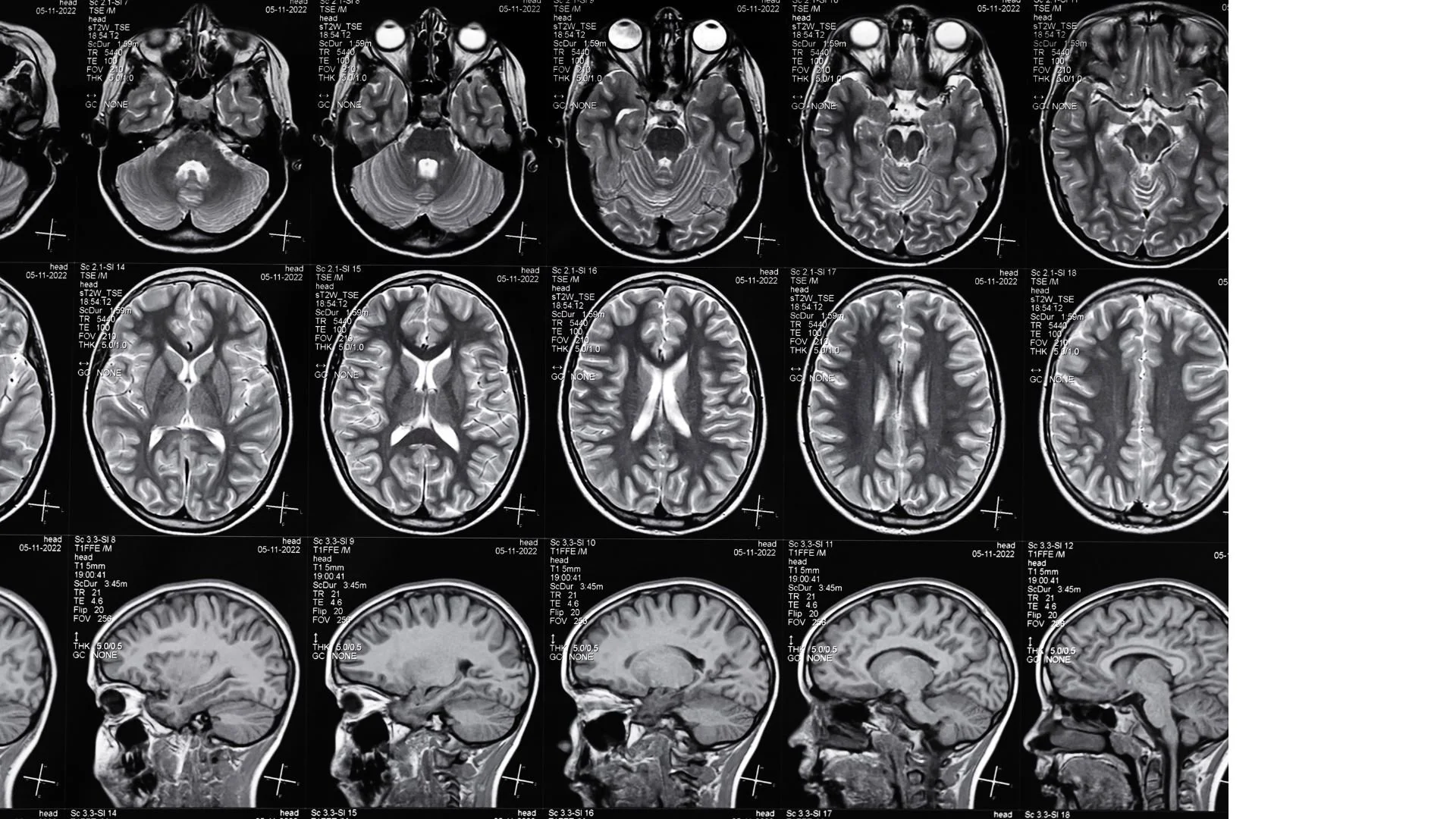
When to see a doctor: Always seek medical attention if a head injury causes any loss of consciousness, confusion, or other neurologic symptoms. Even if someone felt fine right after hitting their head, if symptoms like headache or dizziness appear later or worsen, get evaluated. Emergency signs requiring 911 or immediate ER visit include: one pupil larger than the other, cannot wake the person, seizure, repeated vomiting, or any of the severe symptoms described. With head injuries, it’s better to be safe and get checked. A healthcare professional might do a neurological exam and possibly a brain scan (CT scan) to see if there’s bleeding or swelling. Remember: a mild TBI can be subtle – the person might just “not feel like themselves.” Trust those observations and get them checked out.
Common Causes of TBI
Traumatic brain injuries result from external force. The most common causes are:
Falls: This is the number one cause of TBI overall, especially in young children and older adults. Examples include falling off a bed or down stairs, slipping in the bathtub, or an elderly person falling due to loss of balance. These can lead to head impacts even from not very high heights, particularly dangerous for seniors who may hit the ground hard.
Vehicle-related collisions: Car accidents, motorcycle crashes, being hit as a pedestrian or cyclist by a vehicle – all are frequent causes of serious head injuries. In a car crash, even with airbags, the rapid deceleration can make the brain slam against the skull. Seatbelts and airbags greatly reduce risk, but TBIs can still occur (e.g., whiplash motion causing a coup-contrecoup brain injury, or hitting your head inside the car).
Sports injuries: High-impact or contact sports can result in TBIs. American football, soccer, hockey, boxing, rugby, skateboarding, equestrian riding – these have all been associated with concussions or worse. Repeated smaller blows (like heading a soccer ball frequently or multiple sub-concussive hits in football) are also a concern, as they can cumulatively cause damage (e.g., chronic traumatic encephalopathy in the long term). Youth sports have protocols now to remove players with suspected concussion because “playing through” a TBI is dangerous.
Violence: Sadly, assaults are a cause – examples include blows to the head in fights, domestic violence cases (like being struck or shaken), or gunshot wounds to the head. Shaken baby syndrome is a form of abuse where a baby is forcefully shaken, causing brain injury; it’s a severe TBI in infants and can be fatal or cause permanent damage. Gunshot wounds or stab wounds to the head obviously are severe TBIs (penetrating injuries).
Blast or combat injuries: Among military personnel, explosive blasts are a common cause of TBIs. The pressure wave from an explosion can cause brain damage even without direct impact – the sudden extreme pressure changes seem to disrupt brain function. Additionally, combat situations can involve shrapnel, falls, or collisions that injure the brain.
Other causes can include being struck by falling objects (like on a construction site), or any situation where the head is subjected to trauma (e.g., being violently shaken in a roller coaster malfunction – rare, but theoretically). Any time the head is jolted violently or struck, there’s a risk of TBI.
Preventing TBIs is a big focus of public health: wearing helmets for biking/motorcycling, using seat belts, fall-proofing homes for the elderly (e.g., removing tripping hazards, installing grab bars), and not diving into shallow water (to avoid head/spinal injuries) are all prevention measures. But accidents still happen, so recognizing and properly treating TBIs is crucial.
Emergency Treatment and Acute Care
Immediate response to a suspected TBI can save lives. If you suspect someone has a serious head injury, call emergency services. Do not move someone who’s had a head injury in a trauma (like a car crash) unless they’re in immediate danger, because they might also have a neck/spine injury. Keep them lying down and still. If they’re vomiting, turn them gently to the side to keep the airway clear. If unconscious, check breathing and pulse and begin CPR if necessary.
In the emergency room, assessment is rapid. Doctors check airways, breathing, and circulation first – ensuring the person has oxygen and stable blood pressure, since the brain needs oxygen and blood flow to prevent further damage. They will immobilize the neck until spinal injury is ruled out. A Glasgow Coma Scale (GCS) assessment is done, which scores eye opening, verbal responses, and motor responses to gauge severity – GCS 13-15 is mild, 9-12 moderate, 8 or below severe.
For moderate to severe TBI, initial treatment focuses on preventing secondary injury to the brain. What does that mean? After the primary impact, the brain can swell or bleed, which raises pressure inside the skull (intracranial pressure). High pressure can cut off blood supply to brain tissue. So, ER and ICU teams work to ensure enough oxygen to the brain, maintain blood pressure, and reduce swelling. They might give oxygen via a mask or ventilator, give IV fluids and medications to keep blood pressure stable, and if needed, medications to reduce brain swelling (like mannitol, a diuretic, to draw out fluid). If the patient is agitated or thrashing (which can happen with brain injury), sedation might be used to prevent further harm.
Imaging tests like a CT scan are done quickly to see if there are treatable lesions – such as a blood clot (hematoma) compressing the brain, or a depressed skull fracture – that need surgical intervention.
Surgery: Some injuries require urgent surgery. For instance, if there’s a hematoma (a collection of blood) pressing on the brain, neurosurgeons will perform a craniotomy to remove that blood and relieve pressure. If there’s significant brain bleeding, surgery might be needed to stop it. A severely fractured skull might need repair if bone fragments are pressing into the brain. In extreme cases where swelling is massive, surgeons might remove a portion of the skull (temporarily) to allow the brain space to swell – this is called a decompressive craniectomy. They may also place monitors inside the skull to keep track of intracranial pressure. All these interventions aim to prevent the secondary damage that can occur in the hours or days after the trauma due to swelling or bleeding.
In ICU care for severe TBI, patients might be put on medications like anti-seizure drugs as a precaution – moderate to severe TBI patients have a risk of seizures in the first week, so preventing seizures can avoid additional brain stress. Sometimes, if pressure in the brain remains high, they might induce a temporary coma with medication because an unconscious brain has lower energy needs. Lowering brain metabolism can protect it when blood flow or oxygen is compromised. Each case is unique, and the medical team continuously monitors neurological status.
For mild TBI (concussion): if no concerning findings are present, typically these are treated with rest and observation. Usually no surgery or hospital stay is needed for a straightforward concussion. The person is advised to rest for the first day or two – both physical rest and cognitive rest (limited screen time, work, studying) – and then gradually resume activities as tolerated. Over-the-counter pain relievers may be used for headaches. It’s crucial to avoid a second head injury during recovery, because “second impact syndrome” (a second concussion before the first heals) can be very dangerous. So athletes with concussions, for example, should not return to play until cleared. Follow-up with a doctor ensures that symptoms are improving and that it’s safe to increase activity.
Recovery and Rehabilitation
Surviving the initial injury is the first hurdle; the next phase is rehabilitation, especially for moderate to severe TBIs. Brain injuries can affect a person’s ability to do everyday tasks, so rehab is aimed at helping them regain as much function as possible and learn ways to compensate for any lasting deficits.
Every TBI is different, and recovery can be unpredictable. Some people make rapid and full recoveries, while others have long-term challenges. Recovery typically continues for months or even years, with the fastest gains often in the first six months after injury.
Rehabilitation services might include:
Physical therapy: to improve mobility, muscle strength, balance, and coordination if the injury affected motor control. For example, someone who had weakness on one side of the body (similar to a stroke) will work with a physical therapist on walking, moving safely, and building strength.
Occupational therapy: focuses on regaining the ability to perform daily activities (bathing, dressing, eating, cooking, etc.) and fine motor skills. Occupational therapists also help with cognitive aspects of daily tasks and can suggest adaptive equipment or strategies – like memory aids if short-term memory is a problem, or methods to organize tasks.
Speech and language therapy: if a TBI affected speech or swallowing, or caused cognitive-communication issues, a speech therapist will work on these. They help patients improve clarity of speech, find ways to communicate if speaking is hard (sometimes with assistive devices), and address any swallowing difficulties to ensure safe eating. They also often work on cognitive skills like attention and memory as they relate to communication (for instance, holding a conversation requires memory and focus).
Neuropsychology and cognitive rehabilitation: a neuropsychologist or cognitive therapist assesses specific cognitive functions (memory, attention, problem-solving, processing speed) and helps the patient practice and improve these skills. They also help with behavioral or emotional changes – for example, if someone has more impulsivity or anger after TBI, therapy can address coping strategies.
Psychological support or counseling: adjusting to life after a brain injury can be emotionally challenging. It’s common for patients to experience frustration, depression, or anxiety as they realize what’s changed. Counseling or support groups can provide emotional support. Also, family therapy or education is often included, since families need to understand the injury and how to help their loved one (and themselves cope).
Recreational therapy: these therapists help people re-engage in hobbies and leisure activities to improve quality of life and provide a sense of normalcy and enjoyment.
Vocational rehabilitation: if the person is able to consider returning to work or school, vocational counselors assess their capabilities and help with strategies or job modifications. They might coordinate gradual return-to-work plans or identify new career options if the old job is not feasible.
Rehab can take place in various settings. Early on, a person might be in an inpatient rehabilitation unit (a hospital-like setting focused on daily intensive therapy). Later, they might continue therapy as an outpatient (visiting therapists a few times a week). The rehabilitation team (which may include a physiatrist, a doctor specializing in rehab medicine) works together to create a plan tailored to the patient’s goals – whether that’s walking without a cane, improving memory to live independently, or being able to return to school.
Coping with a TBI
Recovery is not only physical but also emotional and social. Patients and families often need to adjust to what might be a “new normal,” either temporarily or permanently. Some tips and considerations:
Patience and repetition: The brain heals slowly. Tasks might need to be repeated many times to relearn them. Celebrate small progress.
Structure and routine: A consistent daily routine can help someone with cognitive issues feel more secure and improve function (the brain likes patterns). Keeping items in designated places, using calendars or alarms as memory aids, and taking things one step at a time are helpful strategies.
Avoiding overstimulation: Early on, someone recovering from a TBI might get easily overwhelmed by noise or crowds. A calm, quiet environment during rehabilitation tasks can help concentration. As they improve, they can gradually handle more stimulation.
Support network: Family and friends are crucial. They may need to learn about TBI – for instance, understanding that personality changes or irritability can be a direct result of the injury, not “attitude.” Support groups for TBI survivors and caregivers can provide understanding ears and practical advice (people often share tips on navigating life after TBI).
Preventing future injuries: Once you’ve had one serious head injury, it’s extra important to avoid another. Follow safety measures like wearing helmets, fall-proofing the home, etc., because a second injury could compound damage.
Some people with TBI will make a full recovery and return to their lives as before. Others may have lasting effects – perhaps subtle, like needing more time to process information, or more pronounced, like needing assistive devices to walk or help with daily activities. Every improvement matters. Medical advancements continue as well; for instance, researchers are exploring neuroplasticity (the brain’s ability to rewire itself) and testing treatments like hyperbaric oxygen or new medications to enhance recovery. While there’s no magic cure to instantly fix a damaged brain, the combination of acute care and thorough rehabilitation has led many to regain abilities that initially seemed lost.
Outlook
The outlook for a TBI depends on the severity and the specific injury. Mild TBIs (concussions) usually have an excellent prognosis – symptoms typically resolve within weeks to a couple of months, though a subset of people might experience a post-concussion syndrome with headaches or cognitive symptoms lasting longer. It’s crucial to fully recover before risking another concussion.
For moderate to severe TBI, the outcomes vary widely. Some factors that influence recovery include the area of the brain injured (injuries to certain areas may affect critical functions like speech or movement), the extent of bleeding or time without oxygen, and how quickly treatment was received. Generally, younger brains tend to recover better because of greater plasticity, but older adults can recover too, just possibly more slowly. Rehabilitation can continue to make gains even a year or more after the injury, so it’s an ongoing journey.
Some possible long-term effects of serious TBI include difficulties with memory, attention, or learning; changes in personality or behavior (someone might be more impulsive or have mood swings); trouble with physical coordination or paralysis of limbs; and changes in the senses (like reduced vision or taste/smell). It’s not uncommon for severe TBI survivors to have lifelong challenges, but many can still lead fulfilling lives with the right support and adaptations. Some may not be able to return to their previous occupations but find new ways to be active and involved. Assistive technology (like memory apps, speech devices, wheelchairs, etc.) can greatly improve independence.
In summary, a traumatic brain injury can be a life-altering event, but recovery happens. Early medical care saves lives, and rehabilitation gives back lives – helping individuals maximize their abilities and adjust to any new limitations. Prevention is key: always use safety measures to protect your brain. But if TBI does occur, know that modern medicine and rehab therapy offer hope. Many survivors of TBI and their families often say recovery was a hard road, but with time, effort, and support, they achieved milestones they never thought possible in the early days after the injury. The human brain and spirit are resilient – with the proper care, a person with TBI can continue to improve and find joy and meaning in life.
Please note: This information is provided for educational purposes only and is not a substitute for professional medical advice. Always consult your primary care physician or a qualified healthcare provider regarding any questions or concerns about your health. Content created with the assistance of ChatGPT to provide clear, accessible medical condition descriptions.